Virtual care and remote monitoring is “a huge, evolving field for the nursing profession,” says Jennifer Lounsbury – a registered nurse and nurse practitioner – who is acting operating manager for PHRI’s trial, PVC-RAM-1. In fact, the study’s leadership team is an inter-professional group of registered nurses and physicians working closely with researchers including principal investigators, site leads and project officers.
Video conferencing
“One of the first things you learn in nursing school is to assess the patient through observation,” notes Lounsbury, who is Chief of Inter-professional Practice for oncology, critical care and palliative care for two Hamilton Health Sciences (HHS) hospital sites.
“Video conferencing makes this possible, and our nurses are finding that they are able to build therapeutic, trusting relationships with patients through technology,” Jennifer says.
Remote patient monitoring

At-home monitoring
Nurses conduct secure virtual video visits with patients at home using the Cloud DX technology in the PVC-RAM-1 (post-discharge after surgery using virtual care with remote automated monitoring) study.
Nurses also assess the biophysical data patients have measured (and entered on a tablet) themselves using remote monitoring equipment they were trained on and sent home with from the hospital. The data is transmitted wirelessly to the nursing station at the hospital sites, where nurses monitor these vital signs and can identify if the patient needs further follow-up.
HHS nurses participating in the study – from hematology, intensive care, emergency medicine and other specialties – didn’t necessarily have the technology skills when they arrived for training, but they brought a breadth of patient-care experience and were able to learn the technology quickly.
Research accelerated by the pandemic
The pandemic was the impetus for starting the PVC-RAM-1 study, to find a way that more people can leave the hospital sooner, specifically surgical patients, as well as reduce or eliminate unplanned hospitalization or emergency department visits for these patients.
“The pandemic is just the tip of the iceberg, in terms virtual care’s potential, and how healthcare can be transformed,” notes Carley Ouellette, RN, who is the research project nursing officer on PVC-RAM-1.
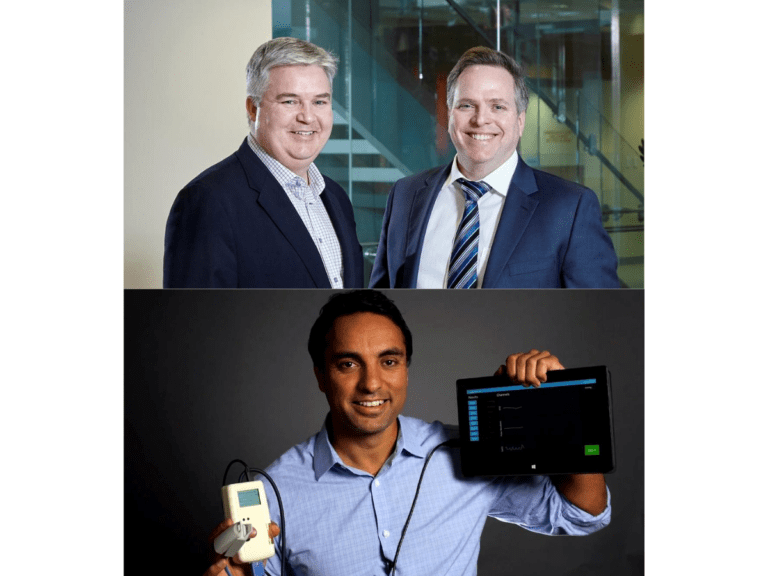
This isn’t the first time Carley has worked on a study with PHRI scientists. A PhD student at McMaster’s school of Nursing with research interests in digital health solutions, she helped PJ Devereaux and Michael McGillion on their previous study, SMArTVIEW.
(Carley is shown here, in 2018, with some of the wearable technology used to measure patients’ health remotely in SMArTVIEW).
Virtual care: shared responsibility
Nurses in the PVC-RAM study also have access to a dedicated physician team that helps support and provide care to patients recovering at home. These physicians can also do a three-way video-call with the patient and nurse if needed.
“It’s very much a shared responsibility model, and the collaboration between MDs and RNs has been instrumental to its success,” Carley says. “We’ve already seen many examples where virtual care has helped address serious postoperative complications that might have led patients back into hospital.”
Michael McGillion, co-PI on PVC-RAM-1, Assistant Dean of Research at McMaster’s School of Nursing and a PHRI Scientist, notes that “frontline nurses have the opportunity to lead the charge in terms of virtual care from hospital to home, in collaboration with physicians and allied health colleagues.”
Story contributed by: Lise Diebel, Hamilton Health Sciences