COVID-19 Research at PHRI
From the international ACT COVID-19 program, to sub-studies PURE SARS-CoV-2 and ACT COAG, and virtual care in the PVC-RAM study
- Homepage
- >
- Special Initiatives
- >
- COVID-19 Research at PHRI
Starting in April 2020, PHRI was quick to design and implement clinical trials and studies to address the COVID-19 pandemic and – just as importantly – our research program has been flexible, with adaptive intervention arms, adaptive therapies and sample sizes to accommodate new and emerging data from research around the world.
As well as investigating therapies that may slow the progression of the disease, PHRI researchers are tackling unique elements, including:
- Why do some people get COVID-19 while others don’t, even with similar degrees of exposure?
- Does ethnicity play a part in getting COVID-19 or in how the disease progresses?
- What underlying co-morbidities are risk factors in getting sick, or being sicker, with COVID-19?
- What are the long-term health effects of the disease, whether or not one gets severe symptoms??
- Does blood clotting play a part in the progression of COVID-19?
- How might the connection between the AC2 receptor and the SARS-CoV-2 virus affect the disease?
- Can remote monitoring of post-surgery patients reduce the burden on hospitals dealing with the pandemic?
ACT COVID-19
The Anti-Coronavirus Therapies to Prevent the Progression of COVID-19 (ACT COVID-19) study includes outpatient and inpatient open-label, parallel group RCTs. More than 100 locations and 4000 patients are expected in this global research program.
ACT-COAG
Our substudy, Assessing Coagulation Biomarkers to Accelerate the Discovery of Effective Therapies for COVID-19 (ACT-COAG), will measure blood clotting markers in patients in our ACT COIVD-19 research program to provide insights into the mechanisms of COVID-19 and its clotting complications, and more.
PVC-RAM-1
The Post Discharge After Surgery Virtual Care with Remote Automated Monitoring Technology (PVC-RAM-1) study investigated if, during the first 30 days following a semi-urgent, urgent or emergency surgery, the effect of RAM technology has on hospital readmission and ER visit, COVID-19 infection, and more.
PURE COVID-19
Are there factors that increase the risk of people getting infected by COVID-19, or that protect against infection? What are the long-term health effects of getting infected by COVID-19? If you’ve had the infection (even if symptoms were not severe), can that lead to long-term lung damage and other complications such as pneumonia, heart attacks, heart failure and stroke? Our substudy, PURE COVID-19, will address this important questions.
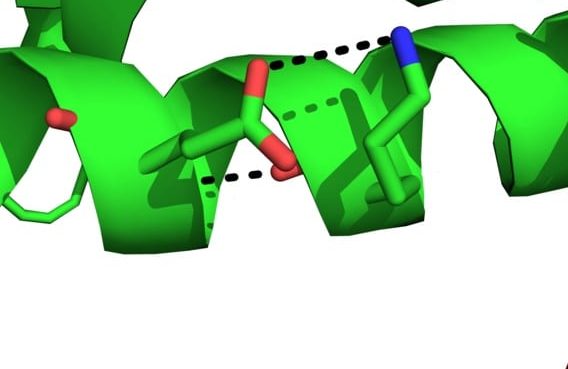
ACE2 and SARS-CoV-2
PHRI’s team in the Genetic and Molecular Epidemiology Laboratory is going deeper with its pre-pandemic investigation into the ACE2 receptor, now that it has been found to be interconnected with SARS-CoV-2.
TIMING
The TIMING study is addressing the marked and unexpected reduction in the supply of the mRNA vaccines to Canada, as of January 2021, which has led to a policy change of delaying the second dose of the Pfizer vaccine to healthcare workers (HCW) up to 35 to 42 days.
We therefore propose an opportunistic study in which we will study and address the following questions:
- What are the cellular immune responses and humoral responses to the first dose of mRNA vaccine up to 42 days and following the second dose up to 12 months?
- How does the dosing schedule impact on the secondary immune responses and long term immunity?

COVID CommUNITY - South Asian
The COVID CommUNITY – South Asian study is being conducted to understand the immune response to the COVID-19 vaccine and its safety in South Asians (people from India, Sri Lanka, Pakistan, Nepal, Bangladesh), who have been disproportionately affected by the pandemic and have worse outcomes from COVID-19 infection compared to other groups.
The study also aims to understand why some people may be less confident in getting the COVID-19 vaccine, and the overall impact of COVID-19 in this community. The study will provide insight into how a pandemic of this scale can be prevented in the community and vulnerable populations.
A total of 3000 participants are being recruited in the Greater Toronto Area and the Greater Vancouver Area.

COVID CommUNITY - First Nations
The COVID CommUNITY – First Nations study is being conducted at several First Nations communities across Canada, to understand the immune response and safety of the COVID-19 vaccine in First Nations people who have been disproportionately affected by the pandemic, and have worse outcomes from COVID-19 infection compared to other groups.
The study also aims to understand why some people are not as confident in the COVID-19 vaccine as others, and to document the overall impact of COVID-19 in these communities.
The study will also provide insight into how a pandemic of this scale can be prevented in these communities and other vulnerable populations.

Key Team Members


Salim Yusuf
Founder and Emeritus Executive Director, Senior Scientist
Salim Yusuf is an internationally renowned cardiologist and epidemiologist, whose work over 40 years has substantially influenced prevention and treatment of cardiovascular disease. Medically qualified from St John’s Medical College in Bangalore in 1976, he received a Rhodes Scholar-ship and obtained a DPhil from Oxford, during which he (along with Richard Peto, Rory Collins and Peter Sleight) initiated the concepts of large, simple trials, and meta-analysis. He coordinated the first ISIS trial (which established the structure for future international collaborative work in cardiovascular and several other diseases) that demonstrated the value of beta-blockers in myo-cardial infarction, and was a member of steering committees for all subsequent ISIS trials.
In 1984, following clinical training in medicine and cardiology in the UK, he moved to the National Institutes of Health, Bethesda, USA, where he led the SOLVD trial (establishing the value of ACE-inhibitors on LV dysfunction) and DIG trial (clarifying the role of digitalis).
In 1992 he moved to McMaster University as head of cardiology, where he established an inter-national program of research in cardiovascular diseases and prevention, culminating in the creation of the Population Health Research Institute. His therapeutic trials have established the roles of ACE-inhibitors in CVD prevention, dual antiplatelet therapies in acute coronary syndromes, novel antithrombotic therapies, and most recently the value of the polypill in substantially pre-venting heart attacks and strokes globally, and at low cost. The Polypill was recently included by the WHO in its Essential Medicines List.
His epidemiologic work in over 80 countries involving all inhabited continents of the world shows the majority of risks of both heart attacks and strokes are attributable to a few risk factors. He currently leads the PURE study exploring the role of societal and environmental factors in CVD. This study (PURE) involves 200,000 people from over 800 communities in 27 high, middle and low-income countries.
He has built capacity for clinical and population research across Canada and the world by establishing research networks involving over 1500 sites in 102 countries. He has trained over 100 researchers, many of whom are now nationally or internationally renowned leaders in medical research. He has helped develop major research institutes or programs in Canada, India, Argentina, Brazil, S. Africa, Saudi Arabia, Malaysia, and China.
He holds a Heart and Stroke Foundation of Ontario Research Chair, was a Senior Scientist of the Canadian Institutes of Health Research (1999-2004), and has received (among over 100) the Lifetime Research Achievement award of the Canadian Cardiovascular Society and the World Heart Federation, the Paul Wood Silver Medal of the British Cardiac Society, the European So-ciety of Cardiology gold medal, the American Heart Association Clinical Research Award, the Killam Prize, and the Canada Gairdner Wightman Award in 2014. He has been inducted into the Royal Society of Canada, been appointed an Officer in the Order of Canada, and has been in-ducted into the Canadian Medical Hall of Fame in 2014. In 2023 he was elected as an Honorary Fellow of St. John’s College, Oxford. He has been conferred 4 honorary doctorates.
He has published over 1400 articles, and was the second most cited researcher in the world for 2011, and has been among the highest cited scientists in the world (his H index is currently 17th of all scientists in history) for over a decade. He is Past President of the World Heart Federation, where he initiated the Emerging Leaders program (now named after him) to build capacity for research in all continents of the world, with the aim of halving the CVD burden globally within a generation. This program has already trained over 250 individuals from 50 countries.


John Eikelboom
Senior Scientist
John Eikelboom is Professor, Department of Medicine, McMaster University, Senior Scientist, Population Health Research Institute, Hamilton Health Sciences Corporation, and Hematologist, Thrombosis Service, Hamilton General Hospital. He completed training in Internal Medicine and Hematology in Perth, Australia, in 1998 and in Health Research Methodology at McMaster University, Canada, in 2000.
He has authored or co-authored more than 800 articles in peer-reviewed journals and for the past decade has been listed annually by the Web of Science among the top 1% of cited researchers. He holds the Jack Hirsh/Population Health Research Institute Chair in Thrombosis and Atherosclerosis. His current research, supported by peer reviewed funding from the Canadian Institutes for Health Research and the Gates Foundation focuses on the efficacy and safety of antithrombotic therapies in arterial, venous, cardiac, and procedure-associated thromboembolism as well as strategies to reduce the burden of the “big three” infectious diseases (HIV, TB, malaria) on the African continent.


PJ Devereaux
Deputy Director, Senior Scientist
Devereaux is a cardiologist, perioperative care physician, and clinical epidemiologist. He is the Director of the Division of Perioperative Care at McMaster University and a Deputy Director, Senior Scientist, and Scientific Leader of the Anesthesiology, Perioperative Medicine, and Surgical Research Group at PHRI. He is the Nominated Principal Applicant of the Accelerating Clinical Trials (ACT) Consortium, which is the Pan-Canadian Clinical Trials Consortium funded by the Canadian Institutes of Health Research (CIHR). Additionally, he holds a Tier 1 Canadian Research Chair in Perioperative Medicine.
Devereaux is a full Professor at McMaster University and the President of the Society of Perioperative Research and Care. He has published over 450 peer-reviewed papers and more than 85 book chapters, editorials, and commentaries, including 17 in the New England Journal of Medicine, 13 in the Lancet, and 11 in JAMA. He has an h-index of 115 and has given over 1000 lectures and research presentations in 41 countries. His research program focuses on major vascular complications during and after surgery, and he has led many large international randomized trials and prospective cohort studies on this topic.


Guillaume Paré
Director, CRLB- GMEL; Senior Scientist
Guillaume Paré is Director of the Clinical Research Laboratory and Biobank (CRLB) – Genetic and Molecular Epidemiology Laboratory (GMEL) and Senior Scientist at the PHRI. He is also Deputy Director of the Thrombosis and Atherosclerosis Research Institute (TaARI), a Professor of Pathology and Molecular Medicine, a Professor in the Department of Health Research Methods, Evidence and Impact, and a University Scholar at McMaster University. A medical biochemist with board certification from the Royal College of Physicians and Surgeons of Canada, Gui completed a Master’s in Human Genetics at McGill University under the supervision of renowned geneticist Thomas Hudson. He further trained in genetic epidemiology with Paul Ridker at Harvard Medical School.
His clinical interests are centered on lipoprotein disorders, obesity and cardiovascular disease prevention, with research interests in cardiovascular genetics, biomarker development and pharmacogenomics. Gui’s research combines high-throughput biomarker screens with genetics, bioinformatics and epidemiology to identify novel cardio-metabolic biomarkers. He has published more than 300 original contributions in peer-reviewed journals, all related to his research program in cardiometabolic disease and genetics. These include first or last authored articles in the NEJM, Lancet, Nature Communications, Circulation, EHJ, Stroke, JACC, PloS Genetics, Circulation Genomics and Precision Medicine and AJHG. His work has been sited over 45,000 times with a corresponding h-index of 89. He was inducted to the Royal Society of Canada’s College of New Scholars, Artist and Scientists in 2018.


Sonia Anand
Senior Scientist
Sonia Anand is a Professor, Medicine and Epidemiology at McMaster University; Associate Chair, Diversity and Equity in McMaster’s Department of Medicine; Director of McMaster’s Population Genomics Program; inaugural Chair, Equity, Diversity and Inclusion (EDI) Committee of the Canadian Cardiovascular Society; and Director, Chanchlani Research Centre for Global Health at McMaster, among other roles.
Her present research focuses upon the environmental and genetic determinants of vascular disease in populations of varying ancestral origin, women and cardiovascular disease. Sonia has published more than 200 articles in peer review journals. Shas been inducted into the Canadian Academy of Health Sciences, and received the Queen Elizabeth II Diamond Jubilee Medal.


Hertzel Gerstein
Interim Executive Director; Senior Scientist
Hertzel Gerstein is PHRI’s Interim Executive Director and Senior Lead of the Diabetes Scientific Program. He is also a Professor of Medicine at McMaster University where he holds the Population Health Research Institute Chair in Diabetes; an Endocrinologist; Director of the Boris Clinic Diabetes Care and Research Program; Chair of Diabetes Clinical Trials Network Canada; and a Fellow of both the Canadian Academy of Health Sciences and the Royal Society of Canada.
Gerstein pioneered and firmly established international long-term diabetes-focused outcomes trials as the norm to support Evidence-Based Diabetes Care. Randomized trials that he designed and led have collectively included more than 90,000 people with either diabetes or prediabetes to date, and have studied and identified clinically important, life-saving diabetes therapies. These trials were supported by the US National Institute of Health, the Canadian Institutes of Health Research, other Canadian peer-review agencies, and by industry. Together, they have substantially expanded the evidence-base pertaining to the prevention, remission, and treatment of diabetes and its consequences, and some of their findings have provided the evidence base for international diabetes guidelines and novel drug indications that have improved the lives of people living with diabetes or prediabetes.
His research has been published in over 600 papers and his h index is 100. His work has been recognized by many awards, including the 2012 Canadian Diabetes Association’s Lifetime Achievement Award and the 2022 American Diabetes Association’s Outstanding Achievement in Clinical Diabetes Research Award.


Darryl Leong
Senior Scientist
Leong’s clinical interests include cardio-oncology, frailty, multi-morbidity, and echocardiography. He is the Director of the McMaster University and Hamilton Health Sciences Cardio-Oncology Program. Leong graduated from the University of Adelaide Medical School with Deans Listing and Honours for academic excellence in 2000. He completed his cardiology training, Doctor of Philosophy, Master of Public Health, and Master of Biostatistics degrees at the University of Adelaide, Australia. He has completed a fellowship in cardiovascular imaging at the Leiden University Medical Centre, the Netherlands, before relocating to Canada.
Leong is an Associate Professor in the Division of Cardiology, Department of Medicine, at McMaster University and Hamilton Health Sciences. His research is supported by the Canadian Institutes of Health Research, Canadian Cancer Society, and the United States Department of Defense, among others. He has published approximately 200 manuscripts, including leading publications in the Lancet and New England Journal of Medicine as well as top cardiovascular journals. He is a Clinician Scientist of the Heart and Stroke Foundation of Canada and has received the Clive Kearon Mid-Career Award from McMaster University. Additionally, he serves as the Director of the Internal Medicine Resident Research Program and the Cardio-Oncology Program at McMaster University.


Michael McGillion
Scientist
Michael McGillion is Associate Professor, and Assistant Dean, Research, at the School of Nursing, McMaster University. He is the Heart and Stroke Foundation/Michael G. DeGroote Endowed Chair in Cardiovascular Nursing Research, and the International Visiting Professor of Digital Health, at Coventry University in the UK.
He is an internationally-recognized researcher in the area of persistent forms of cardiac pain such as refractory angina and unrelieved chest pain following successful revascularization procedures. He was Chair of the Joint Canadian Cardiovascular Society – Canadian Pain Society guidelines for the management of refractory angina, funded by the Canadian Institutes of Health Research (CIHR). He is Principal Investigator of the largest CIHR-funded, international prospective cohort study to examine social and psychological predictors of chronic post-surgical pain following cardiac surgery. His research focuses on remote automated monitoring and virtual recovery support for people recovering from cardiac and vascular surgery, decision support for people living with RFA, and global-scale, web-based dissemination of new evidence on persistent forms of cardiac pain.
Mike has been recognized for his research and advocacy by receiving the Canadian Pain Society Early Career Award and the McMaster University Arch Award for outstanding contributions to society; and was the first University Scholar (2019) from the McMaster School of Nursing.


Richard Whitlock
Senior Scientist
Richard Whitlock is Associate Chair, Research, and a Professor at the Department of Surgery, McMaster University. He was awarded the inaugural Canada Research Chair in Cardiovascular Surgery in 2020.
As well as being a PHRI Scientist, Richard is a cardiac surgeon and intensive care physician at Hamilton Health Sciences. His clinical focus is on aortic valve intervention and aortic surgery. He is a lead investigator for the CIHR funded studies SIRS, LAAOS III, and TRICS III, which have established a network of more than 120 centres to address important questions in his field.
He has published more than 90 articles in referred journals. Medically qualified at the University of Toronto, Richard received his specialist training in cardiac surgery and critical care medicine at McMaster University. In 2012, he received his PhD in clinical epidemiology.


Sanjit Jolly
Senior Scientist
Sanjit Jolly is an interventional cardiologist at Hamilton Health Sciences and associate professor at McMaster University. He has formal training in clinical trials with a M.Sc. in Health Research Methodology from McMaster. He was the principal investigator of the RIVAL trial, a randomized trial of 7021 patients comparing radial and femoral access for coronary intervention. He is also the principal investigator trial of the ongoing TOTAL trial, an international randomized trial (N=10,700) of thrombectomy during primary PCI.


Emilie Belley-Côté
Associate Deputy Director, Scientist
Emilie Belley-Cote obtained her MD from Université de Sherbrooke. After internal medicine and cardiology training, as well as an MSc in Clinical Sciences – research profile at Université de Sherbrooke, she completed a critical care fellowship at McMaster University. In 2019, she completed a PhD in Health Research Methodology at McMaster University. She is now an associate professor in the Department of Medicine at McMaster University; she practices critical care cardiology in the cardiovascular intensive care unit and coronary care unit at the Hamilton General Hospital. Her research interests include perioperative cardiac surgery care, knowledge synthesis and guideline development. At this stage in her career, she leads the CIHR-funded LIMIT, DANCE and PRINCE trials. She has over 300 publications, including articles in NEJM, Lancet, JAMA, as well as first tier critical care journals.
MyLinh Duong
Associate Scientist
MyLinh Duong is a respirologist at Hamilton Health Sciences, and Associate Professor, Department of Medicine, McMaster University. Her research interests include respiratory epidemiology, and understanding the environmental and social determinants of lung development and lung function. She is the respiratory lead for a number of PHRI’s population-based studies including PURE, FAMILY and the global heart failure registry, G-CHF.
She obtained her medical degree, specialist and sub-specialist training in Internal Medicine, Sleep Medicine and Respiratory Medicine at the University of Adelaide, Australia. This was followed by a research fellowship in the areas of airway inflammation, asthma and COPD at the Firestone Clinic and McMaster University, Canada, where she obtained a Master’ degree in Health Research Methodology and Epidemiology.


Noel Chan
Scientist
Noel Chan is an Assistant Professor in the Division of Hematology and Thromboembolism, Department of Medicine, McMaster University, specializing in anticoagulant therapy and thrombosis medicine. His research seeks to improve our understanding of the triggers for thrombosis (including the role of inflammation) and the determinants of variable response to antithrombotic therapies to inform on novel strategies that have the potential to further reduce the burden of thrombosis.


Dominik Mertz
Scientist
Dominik Mertz is Associate Professor, Division of Infectious Diseases, Department of Medicine, McMaster University, and Medical Director Infection Control at Hamilton Health Sciences. His research interests include the epidemiology and risk factors for resistance and infections by resistant bacteria; prevention of C. difficile infection; infection control and of hospital epidemiology; and antimicrobial stewardship.
He has published more than 60 peer reviewed articles to date, is an associate editor for BMC Infectious Diseases, and serves as the first-named editor for the third edition of the book ‘Evidence-based Infectious Diseases’.


Sumathy Rangarajan
Program Director
Sumathy Rangarajan has been Program Director, Global Health, since 2016, preceded by many years’ service at PHRI in other roles. She oversees the PURE study team, as well as the INVICTUS rheumatic AF treatment trial, the CANPWR pediatric weight management registry, and others.
She holds both a Bachelor of Science Degree and a Master of Science degree from Pune University in India.


Dipika Desai
Program Manager
Dipika Desai oversees many epidemiologic studies, including the South Asian birth cohort, START, the South Asian Heart Risk Assessment (SAHARA), and the Canadian Alliance for Healthy Hearts and Minds (CAHHM), as well as management assistance and oversight in the utilization of samples from a number of other studies.
She has a Bachelor’s degree in Food and Nutrition from the M S University in Baroda, India, and a Master’s degree in Human Nutrition from the University of British Columbia.


Jessica Vincent
Head of Operations
Jessica Vincent has more than 15 years’ experience in coordinating and managing large, international clinical trials. She holds an Honours Bachelor of Science Degree from Queens University, and a Master of Clinical Epidemiology Degree from the University of Newcastle.


